Dementia screening for all
Patient-focused collection of information
Are DMDs here to stay?
Advancing the clinical care pathway
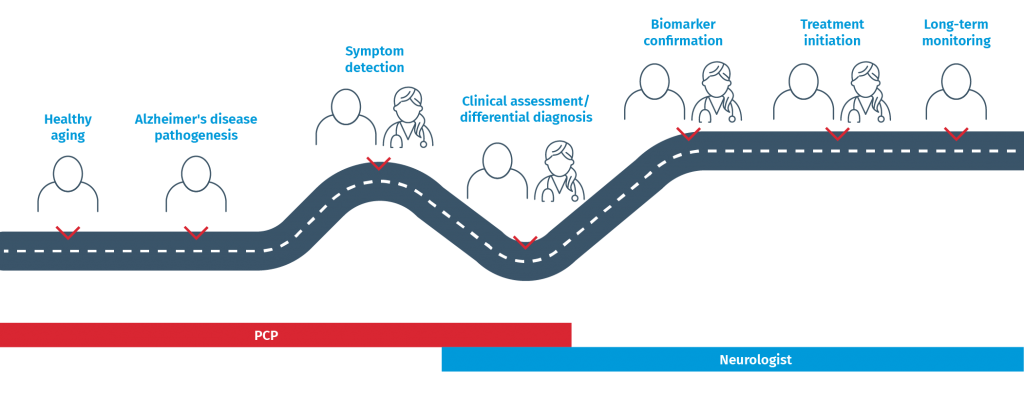
As more patient information is collected along this pathway, being able to collate it all in one location and make sense of it all is the next challenge. Software tools, such as our cDSI™ application, provide clinicians with a single source of information as well as AI-driven insights from that information. This will become more important with new developments, such as collecting and incorporating data from gait analyses and other apps to support a dementia analysis, that we heard about from some conference attendees. Given that one of the barriers to a timely and accurate Alzheimer’s diagnosis presented in the Lilly-sponsored symposium is a lack of physician confidence in differentiating between dementias and issuing a diagnosis, tools that support an accurate diagnosis are important.
- Making available validated, easy-to-use tools that help with screening and diagnosis
- Educating patients, caregivers and clinicians about the need for an earlier diagnosis and how that can be accomplished
- Create awareness for the early detection and management
- Spread the word about the benefits of the collaborative clinical care model
- Integrate passive digital markers, patient-reported outcomes, and caregiver-reported outcomes to improve the process of early detection in primary care
- Expand the processes for early detection into the patient’s home and community via digital solutions
