Clinicians value tools that can help them confidently diagnose dementias.

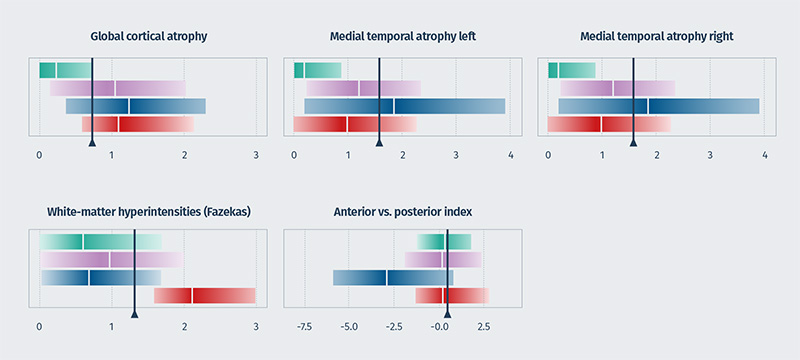
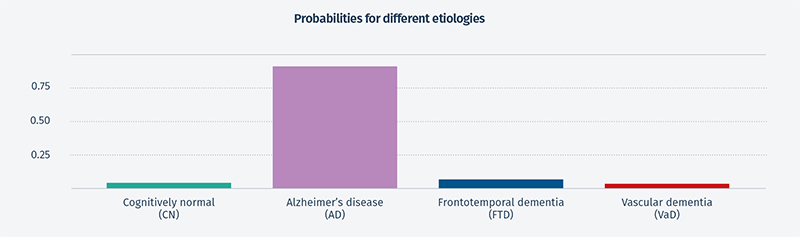
The report is based on MRI data only, using our cDSI™ application’s proprietary machine learning method that measures the similarity of the following disease-specific imaging biomarker values from the patient to those of different diagnostic groups:
- Cortical atrophy score/global cortical atrophy (GCA) score
- Hippocampal atrophy score/medial temporal atrophy (MTA) score
- White matter hyperintensity (WMH) volume/Fazekas score
- Anterior vs posterior index
Applying artificial intelligence to neuroradiology requires a multidisciplinary approach.
Although clinicians don’t need to understand the development process or the science and technology behind the outputs, they do want to know the system has been validated. This was a question of interest regarding our new report from neuroradiologists at our booth. Collaborating with clinicians from memory clinics, we have been able to show 76% accuracy in separating AD, FTD, VaD, and normal cognition using MRI data in cDSI, which is much higher than other methods. The remaining 24% of cases comprised mixed dementia diagnoses and pre-clinical disease, among others. For the 50% of patients with the highest probability, the accuracy increased to 88%. When additional patient variables were added to cDSI, such as cognitive test results, cerebrospinal fluid test results, and genetic test results, the diagnostic accuracy increased to 88% for all patients and 99% for the 50% of patients with the highest probability.
We’re looking forward to next year.
We had meaningful conversations during ASNR22 with a number of neuroradiologists whose specialties align with our focus on neurodegenerative diseases, including dementias, MS, and traumatic brain injuries and who are interested in the latest developments to improve their practice. The strong audience, combined with the academic nature of the conference, contributed to a positive, high-value experience, and when asked if we’ll attend again next year, our answer is “Absolutely.”
